Endometriosis: Symptoms, Causes, Diagnosis & Treatments
What Is Endometriosis?
Endometriosis is a chronic condition where tissue resembling the lining of the uterus (endometrium) grows outside the womb, often in the pelvic region, lower abdomen, and, in rare cases, other parts of the body. While researchers don’t yet fully understand what causes endometriosis, contributing factors may include genetics, immune system issues, and hormonal imbalances.
This condition affects individuals assigned female at birth, though some patients may identify as transgender men. Healthcare providers should always respect a patient’s gender identity and chosen pronouns. Endometriosis in transgender men will be discussed later in this article.
How Common Is Endometriosis?
Endometriosis affects an estimated 10% to 18% of women of reproductive age, though many cases go undiagnosed due to mild or absent symptoms. The condition is significantly more common among women experiencing chronic pelvic pain or infertility, with prevalence rates rising to 30-50% in these groups. In fact, endometriosis is one of the leading causes of fertility issues, second only to uterine fibroids as a common gynecological condition.
Diagnosing endometriosis can be challenging because it often requires confirmation through laparoscopy. The average age of diagnosis is around 28, but it can also occur in teenagers and, in rare instances, younger girls.
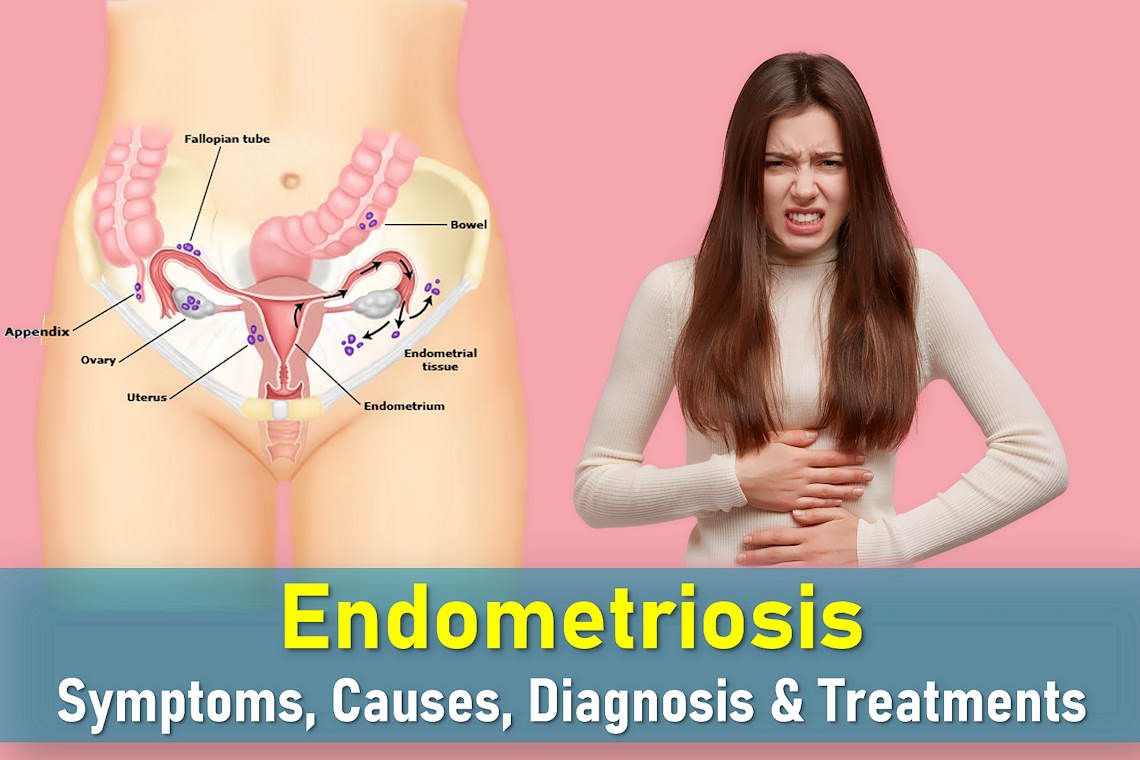
Common Locations of Endometrial Tissue Implants
Misplaced endometrial tissue, known as implants, can develop in various areas, including:
- Ovaries
- Uterine ligaments
- The peritoneum (abdominal and pelvic lining)
Less common sites include:
- Fallopian tubes
- Outer surfaces of the intestines
- Bladder and ureters
- Space between the vagina and rectum
In rare cases, endometriosis may spread to the lungs, heart sac, vulva, cervix, or surgical scars.
Endometriosis Stages
Doctors classify endometriosis into four stages based on the location, extent, and depth of the endometrial-like tissue:
- Stage 1 (Minimal): Few superficial implants
- Stage 2 (Mild): More implants but still limited
- Stage 3 (Moderate): Deep implants with possible ovarian cysts
- Stage 4 (Severe): Widespread deep implants and large cysts
It’s important to note that the stage doesn’t always correlate with symptom severity. Some women with stage 4 endometriosis experience minimal discomfort, while others with milder cases may have significant pain. This variability makes personalized treatment essential.
How Does Endometriosis Affect the Body?
Like normal uterine tissue, these implants respond to hormonal changes during the menstrual cycle, leading to bleeding, inflammation, and endometriosis pain. Symptoms vary widely, some women experience severe discomfort, while others may have no noticeable signs. Over time, the misplaced tissue can grow and spread, though progression rates differ from person to person. In some cases, it remains superficial, while in others, it penetrates deeply, forming nodules.
Endometriosis Symptoms
The symptoms of endometriosis vary widely, some women have no symptoms at all, while others experience mild to debilitating discomfort. Interestingly, symptom severity doesn’t always correlate with the size or extent of endometrial implants. Some women with large patches have no pain, while others with small lesions struggle with severe symptoms. Pain perception can also differ based on cultural background, ethnicity, or neurodiverse conditions.
Common Symptoms of Endometriosis
- Painful periods (dysmenorrhea): Unlike typical menstrual cramps, endometriosis pain often starts days before bleeding and may persist throughout the cycle. Over time, this discomfort can become chronic, lasting most of the month.
- Pain during or after sex (dyspareunia): Deep pelvic pain during intercourse is common, sometimes lingering for hours afterward.
- Fertility challenges: Up to 50% of women with infertility have endometriosis. While blocked fallopian tubes may explain some cases, the link isn’t always clear.
- Other symptoms: Fatigue, painful bowel movements, lower back pain, and urinary discomfort. Rarely, blood appears in urine or stool.
- Unusual symptoms: In rare cases, endometrial tissue growing in distant areas (like the diaphragm) can cause cyclical nosebleeds or shoulder pain coinciding with periods.
Endometriosis Risk Factors
Endometriosis affects millions of women in the U.S., but some individuals face a higher risk due to genetic, hormonal, and lifestyle factors. Research suggests that certain conditions may increase the likelihood of developing endometriosis, while others may help lower the risk.
Factors That Increase Endometriosis Risk
If you’re wondering what causes endometriosis, studies point to several key risk factors:
- Family history: Having a mother, sister, or daughter with endometriosis raises your risk, suggesting a possible genetic link.
- Uterine abnormalities: An irregularly shaped uterus, as diagnosed by a doctor, may contribute to the condition.
- Early menstruation: Getting your first period before age 11 is associated with higher risk.
- Short menstrual cycles: Cycles averaging fewer than 27 days may increase susceptibility.
- Heavy periods: Menstrual bleeding lasting longer than seven days appears linked to endometriosis development.
Potential Protective Factors
Some factors may help reduce endometriosis risk:
- Pregnancy and breastfeeding: These hormonal changes may temporarily suppress endometriosis symptoms.
- Later menstruation: Getting your first period after age 14 correlates with lower risk.
- Dietary choices: Some studies suggest citrus fruits and other antioxidant-rich foods might play a protective role.
What Causes Endometriosis?
While the exact causes of endometriosis remains unclear, several theories attempt to explain its development:
- Retrograde menstruation: One leading theory suggests that during menstruation, some endometrial cells flow backward through the fallopian tubes into the pelvic cavity, where they implant and grow.
- Adhesions and cysts: These misplaced cells can form “sticky” patches that bind organs together (called adhesions). In some cases, they develop into fluid-filled cysts on the ovaries known as endometriomas or “chocolate cysts” due to their dark, bloody content.
Other potential factors being studied include immune system disorders, genetic predisposition, and environmental triggers, but none provide a complete explanation.
Endometriosis and Fertility
One of the most concerning aspects of endometriosis is its potential impact on fertility. Studies show that 24-50% of women experiencing infertility have endometriosis. The relationship between the two conditions is complex:
How Endometriosis Affects Fertility
- Scar tissue formation: Endometrial lesions can create adhesions that may block fallopian tubes or interfere with egg release.
- Inflammation: The condition creates an inflammatory environment that might affect egg or sperm function.
- Implantation issues: Some research suggests endometriosis could make it harder for fertilized eggs to implant in the uterine lining.
Pregnancy Possibilities With Endometriosis
Many women with endometriosis do conceive, either naturally or with medical assistance. Treatment options like laparoscopic surgery to remove endometrial growths or assisted reproductive technologies (including IVF) have helped countless women achieve successful pregnancies. If pregnancy is among your goals, discuss your endometriosis treatment options with a reproductive specialist.
How Is Endometriosis Diagnosed?
If you are experiencing symptoms suggestive of endometriosis—such as pelvic pain, heavy periods, or infertility—your doctor will follow a structured diagnostic approach. While no single test can definitively confirm endometriosis without surgery, a combination of clinical evaluation and imaging can help guide diagnosis and treatment.
Initial Evaluation
Your healthcare provider will begin with:
- A thorough review of your medical history and symptom patterns
- A pelvic examination to check for cysts, tenderness, or other abnormalities
Diagnostic Tests
To help rule out other conditions and assess for signs of endometriosis, your doctor may recommend:
- Pelvic swabs: Used to exclude infections that can mimic endometriosis symptoms
- Ultrasound imaging: Typically a transvaginal ultrasound for a closer look at reproductive organs
- Can detect endometriomas (ovarian cysts linked to endometriosis)
- May not identify small or superficial endometrial implants
- Blood tests: While not diagnostic, they may help rule out other causes of pelvic pain or abnormal bleeding
Referral to a Specialist
Referral to a gynecologist or endometriosis specialist is often recommended if:
- Symptoms are severe, chronic, or not responding to initial treatments
- First-line therapies are ineffective or not well-tolerated
- A physical exam or ultrasound suggests the presence of endometriosis or related complications
- There is suspicion of bowel, bladder, or ureter involvement
- You are trying to conceive, as some treatments may interfere with fertility
Specialized Diagnostic Tests
Pelvic MRI Scan
MRI may be used in more complex or advanced cases:
- Can help detect deep infiltrating endometriosis, especially when it involves the bowel, bladder, or other pelvic organs
- Not all types of endometriosis are visible on MRI; a normal scan does not exclude the condition
Diagnostic Laparoscopy
Laparoscopy is considered the gold standard for diagnosing endometriosis:
- Performed under general anesthesia with a small incision near the navel
- A laparoscope (thin camera) is inserted to view pelvic organs in detail
- Allows for tissue biopsy and, in many cases, treatment of endometrial lesions during the same procedure
Although minimally invasive, laparoscopy offers the most definitive diagnosis and may significantly improve symptoms when combined with surgical treatment.
Endometriosis Treatment Options
Endometriosis treatment is highly individualized and depends on factors such as the severity of symptoms, the extent of the disease, and whether you are trying to conceive. While some women manage well with medication alone, others may need surgical intervention. The goal is to reduce pain, control the growth of endometrial-like tissue, and improve quality of life.
Pain Management Strategies
For endometriosis pain relief, initial treatment often focuses on managing discomfort with over-the-counter or prescription medications:
- Paracetamol (acetaminophen): Suitable for mild pain, especially when taken regularly during menstruation
- NSAIDs (e.g., ibuprofen, naproxen): Often more effective than paracetamol for cramping and inflammation. Not recommended for individuals with gastrointestinal issues such as ulcers
- Codeine-based medications: Prescribed for more severe pain when NSAIDs are ineffective or contraindicated, but may cause constipation and should be used with caution
- Tranexamic acid: Can help reduce heavy menstrual bleeding, often used in combination with pain relievers
For best results, pain medication should be taken at the onset of symptoms or preemptively during your period, rather than waiting for the pain to escalate.
Hormonal Therapies
Hormonal treatments aim to limit or stop menstruation, which helps slow the growth of endometrial tissue. These endometriosis medication options are often contraceptive in nature.
Combined Hormonal Contraceptives (CHC)
- Available in oral pills, skin patches, or vaginal rings
- Help regulate or eliminate periods, reducing associated pain
- Not suitable for those with a history of blood clots, high blood pressure, or certain types of migraines
Progestogen-Only Options
- Available as daily pills (e.g., norethisterone, dydrogesterone)
- Long-acting forms such as contraceptive implants or depot injections
- Levonorgestrel-releasing intrauterine device (IUD), such as Mirena, which provides localized hormone delivery and long-term symptom relief
Note: Some oral progestogens are not reliable for contraception. If avoiding pregnancy is important, speak with your doctor about the best option for your needs.
Surgical Treatment Options
Surgery may be necessary when symptoms are severe, when endometriomas or other complications are present, or when other treatments are ineffective.
Laparoscopic Surgery
The most common surgical approach for endometriosis:
- Minimally invasive technique using small abdominal incisions
- Allows removal (excision) or destruction (ablation) of endometrial lesions
- Can also treat ovarian endometriomas (also called “chocolate cysts”)
- Often improves pain and fertility outcomes
Laparotomy
An open surgical approach, generally used when:
- Endometriosis is widespread and not manageable with laparoscopy
- Large cysts or deep pelvic adhesions are present
Hysterectomy
In select severe cases, especially for women who have completed childbearing:
- Removal of the uterus (hysterectomy) and sometimes the ovaries (oophorectomy) may be recommended
- This is not a guaranteed cure, as endometrial tissue can still persist or recur
- Oophorectomy leads to menopause and may require hormone replacement therapy (HRT) to manage symptoms
Specialist Medical Therapies
For individuals with advanced or recurrent endometriosis, specialists may prescribe more aggressive hormonal therapies:
- GnRH (Gonadotropin-Releasing Hormone) analogs: Suppress estrogen production by inducing temporary menopause. Effective but can cause menopausal symptoms like hot flashes and bone thinning
- Aromatase inhibitors: Block estrogen production in tissues, used in combination with other hormonal therapies to improve effectiveness
- Danazol: A synthetic androgen that suppresses estrogen but is less commonly used due to side effects such as weight gain, acne, and voice changes
Managing Recurrence
Endometriosis is a chronic condition, long-term management is often necessary. Even after surgery or hormonal therapy, symptoms may return:
- Ongoing treatment may be needed to maintain symptom relief
- Different treatment strategies may be required over time depending on how the disease progresses
- Regular monitoring by your healthcare provider helps track symptom changes and optimize your care plan
Can Endometriosis Be Prevented?
Since endometriosis is an idiopathic condition (meaning its exact cause remains unknown), there are no guaranteed prevention methods. However, recognizing potential signs of endometriosis early and understanding your personal risk factors can help you seek timely medical advice. Maintaining overall reproductive health through regular check-ups may also help with early detection.
Living With Endometriosis
While endometriosis is a chronic condition with no definitive cure, today’s treatment options – from pain management strategies to advanced surgical techniques – can significantly improve quality of life. The key is working with a healthcare provider who specializes in endometriosis care to develop a personalized treatment plan. Remember that symptom tracking, timely medical intervention, and a strong support network can make a meaningful difference in managing this complex condition. With proper care, many women with endometriosis find effective relief and maintain fulfilling lives.
Frequently Asked Questions About Endometriosis
What are the first signs of endometriosis?
The earliest signs of endometriosis often include severe menstrual cramps, chronic pelvic pain, pain during intercourse, and unusual bowel movements during periods. Some women also notice heavy bleeding or fertility challenges.
Can endometriosis affect pregnancy?
While endometriosis can make conception more difficult, many women with the condition successfully get pregnant. Fertility treatments and surgical removal of endometrial tissue can improve pregnancy chances for those struggling to conceive.
How painful is endometriosis?
Pain levels vary greatly – some experience mild discomfort while others have debilitating endometriosis pain that interferes with daily life. The pain often correlates with menstrual cycles but may become constant in advanced cases.
What’s the difference between laparoscopy and other diagnostic methods?
While ultrasounds and MRIs can suggest endometriosis, laparoscopy remains the gold standard for definitive diagnosis as it allows direct visualization and often simultaneous treatment of endometrial implants.
Does endometriosis worsen with age?
Endometriosis typically progresses without treatment but often improves after menopause when estrogen levels drop. However, stage 4 endometriosis can cause permanent damage, making early intervention important.
Are there natural ways to manage endometriosis symptoms?
Some find relief through an endometriosis diet (anti-inflammatory foods), regular exercise, heat therapy, and stress reduction techniques. These complement but don’t replace medical treatments.
Is endometriosis genetic?
Research shows endometriosis often runs in families. Women with a first-degree relative (mother, sister) with the condition have 7-10 times higher risk, suggesting a strong genetic component.