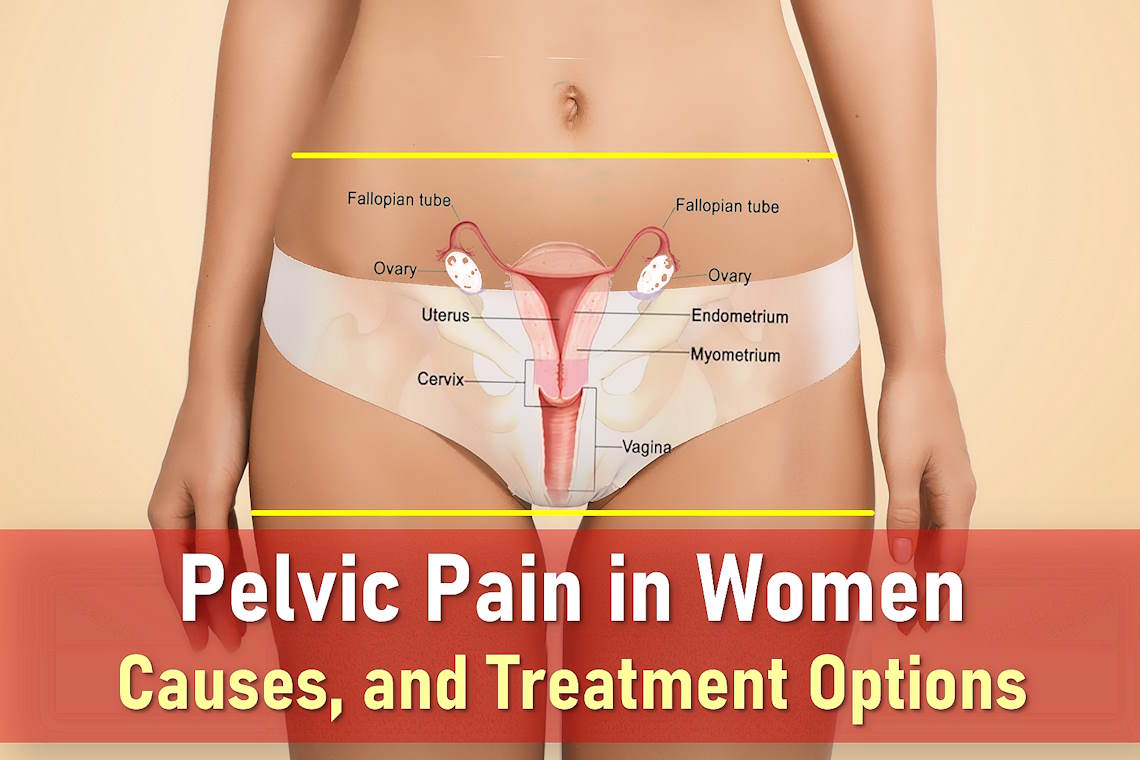
Pelvic Pain in Women: Causes, Treatments, and When to Worry
Pelvic pain is a frequent concern among women, often stemming from various conditions affecting the lower abdomen. This area houses vital organs, including the bladder, intestines, and for women, the reproductive system, uterus, ovaries, fallopian tubes, and cervix. Discomfort in this region can arise from issues with these organs, musculoskeletal problems, nerve-related conditions, or even mental health factors.
The pain may develop suddenly or build gradually, ranging from mild to severe. Some women describe it as a dull ache, sharp stabbing sensations, or cramping similar to menstrual cramps. When pelvic pain persists for more than six months, it is classified as chronic. Additional symptoms may include tenderness, vaginal bleeding or discharge, fever, nausea, or dizziness, depending on the underlying cause.
What Causes Pelvic Pain?
Pelvic pain typically stems from three main sources: gynecological conditions, urinary system disorders, and gastrointestinal issues. Among the most frequent causes are menstrual cramps, urinary tract infections, and irritable bowel syndrome. The pain may range from mild discomfort to severe, debilitating symptoms depending on its origin.
Gynecological Causes of Pelvic Pain
Pelvic pain in women often originates from the reproductive system and may vary in intensity and duration. Some conditions cause cyclic pelvic pain, recurring predictably with menstrual cycles, while others lead to persistent or intermittent discomfort. Accurate diagnosis is crucial as many gynecological conditions share similar symptoms but require different treatments.
Common Gynecological Conditions
- Menstrual Cramps (Dysmenorrhea) – Primary dysmenorrhea involves painful uterine contractions during menstruation, while secondary dysmenorrhea indicates underlying conditions. Symptoms typically include lower abdominal cramping, back pain, and sometimes nausea. Severe cases may require medical intervention.
- Endometriosis & Adenomyosis – Endometriosis occurs when uterine tissue grows outside the uterus, often causing chronic pelvic pain, painful intercourse, and infertility. Adenomyosis involves similar tissue growing into the uterine wall, leading to heavy bleeding and severe menstrual pain that often worsens with age.
- Ovarian Cysts – Most ovarian cysts are harmless, but larger cysts or those that rupture can cause sudden stabbing pain in the pelvic area, bloating, and pressure. Functional cysts typically resolve on their own, while complex cysts may require monitoring or treatment.
- Pelvic Inflammatory Disease (PID) – This infection of reproductive organs often results from untreated STIs and can cause persistent pelvic pain after sex, abnormal discharge, and fever. Left untreated, PID may lead to infertility or ectopic pregnancy.
- Scar Tissue (Adhesions) – Post-surgical adhesions or those from endometriosis/infection can bind organs together, creating chronic pelvic pain syndrome that often worsens with movement or certain activities. Laparoscopic surgery may help severe cases.
- Hydrosalpinx – This condition involving blocked, fluid-filled fallopian tubes often causes dull pelvic pressure or pain. It’s frequently associated with infertility and may require surgical intervention if causing significant symptoms.
- Uterine Fibroids – These benign tumors vary in symptom severity based on size and location. Larger fibroids may cause lower abdominal pain, heavy bleeding, urinary frequency, or constipation by pressing on nearby organs.
Non-Gynecological Causes of Pelvic Pain
Approximately one-third of chronic pelvic pain cases originate outside the reproductive system. Digestive, urinary, and musculoskeletal disorders can all manifest as pelvic discomfort, often requiring different diagnostic approaches.
Digestive System Disorders
- Irritable Bowel Syndrome (IBS) – This functional gut disorder commonly causes lower abdominal pain before bowel movement, bloating, and alternating diarrhea/constipation. Symptoms often improve with bowel movements and may worsen with stress.
- Inflammatory Bowel Disease (IBD) – Crohn’s disease and ulcerative colitis involve chronic intestinal inflammation, potentially causing lower abdominal pain and nausea, bloody stools, weight loss, and fatigue. These conditions require specialized gastroenterological care.
- Constipation or Diverticulitis – Chronic constipation creates pelvic pressure and dull pain, while diverticulitis (inflamed intestinal pouches) causes localized tenderness, fever, and sometimes severe infection requiring antibiotics.
Urinary Tract Issues
- Urinary Tract Infections (UTIs) – These bacterial infections typically cause burning pelvic pain during urination, urgency, and frequency. Kidney involvement may lead to fever and flank pain. Recurrent UTIs warrant urological evaluation.
- Kidney Stones – When stones descend into the lower urinary tract, they can trigger intense, colicky pelvic pain that radiates to the groin, along with nausea and blood in urine. Larger stones may require medical intervention.
- Interstitial Cystitis – This chronic bladder condition involves pelvic pressure, pelvic floor pain, and urinary urgency/frequency without infection. Symptoms often worsen during menstruation and may improve with dietary changes and medications.
Musculoskeletal & Nerve-Related Conditions
- Pelvic Girdle Pain – Common in pregnancy due to hormonal changes and mechanical stress, this condition causes lower back and pelvic pain that worsens with movement. Postural adjustments and physical therapy often help manage symptoms.
- Fibromyalgia – This centralized pain syndrome may contribute to widespread discomfort including pelvic pain, often accompanied by fatigue, sleep disturbances, and cognitive difficulties. A multidisciplinary approach works best for management.
- Nerve Damage (Neuropathy) – Conditions like pudendal neuralgia can cause shooting, burning, or electric shock-like sensations in the pelvis. Causes include trauma, surgery, or compression, and treatment focuses on nerve stabilization.
Pelvic Pain During Pregnancy
Pelvic pain during pregnancy can be a normal part of bodily changes, but it may also signal serious medical issues. Understanding the possible causes helps expectant mothers recognize when to seek medical care:
- Miscarriage: Refers to pregnancy loss before 24 weeks, with most occurring in the first trimester, with signs such as vaginal bleeding (often with clots), lower abdominal or pelvic cramping, and passage of tissue from the vagina.
- Ectopic Pregnancy: A life-threatening condition where the fertilized egg implants outside the uterus, usually in a fallopian tube. Symptoms include sharp or worsening pain on one side, dark vaginal bleeding, and shoulder tip pain from internal bleeding.
- Ruptured Corpus Luteum Cyst: Often harmless but can cause sudden, sharp one-sided pelvic pain and light spotting, especially in the first trimester.
- Preterm Labor: Occurs before 37 weeks and involves regular pelvic contractions, pressure or backache, vaginal fluid leakage, or bloody mucus discharge (“show”).
- Placental Abruption: A serious complication where the placenta detaches from the uterine wall prematurely. Warning signs include sudden severe abdominal or pelvic pain, a firm tender uterus, vaginal bleeding (which may be hidden), and decreased fetal movement.
Psychological Factors in Pelvic Pain
While stress, anxiety, or past trauma don’t directly cause pelvic pain, they significantly influence pain perception and chronicity. The brain-gut-pelvis connection means psychological distress can exacerbate conditions like IBS or chronic pelvic pain syndrome. Integrated treatment addressing both physical and emotional aspects often yields better outcomes.
Emergency Situations Requiring Immediate Care
Sudden, severe pelvic pain that develops abruptly or worsens rapidly may indicate a serious condition needing urgent treatment. Conditions that often require emergency surgery include:
- Appendicitis or intestinal blockage – Can cause severe lower abdominal pain that starts near the belly button and moves to the right side
- Ectopic pregnancy rupture – A life-threatening condition causing sudden stabbing pain in pelvic area and possible fainting
- Ovarian torsion – When an ovary twists, cutting off its blood supply (may cause pelvic pain while pregnant)
- Ruptured ovarian cyst – Can lead to internal bleeding and lower abdominal pain and nausea
- Pelvic abscess rupture – A burst infection pocket in the pelvis
- Bowel perforation or obstruction – Causes intense lower abdominal pain before bowel movement with vomiting
- Aortic aneurysm – A medical emergency causing tearing pelvic bone pain
Danger Signs That Need Prompt Attention
Women experiencing pelvic pain with any of these warning symptoms should seek emergency care:
- Fainting or feeling lightheaded (possible sign of internal bleeding)
- Rapid heartbeat with low blood pressure (indicating shock)
- Sudden, excruciating pain with nausea/vomiting
- Fever or chills (suggesting infection)
- Vaginal bleeding after menopause
When to Schedule a Doctor’s Visit
While not emergencies, these situations warrant medical evaluation within days:
- Postmenopausal bleeding (always requires investigation)
- Persistent or progressively worsening chronic pelvic pain
- Pelvic pain after sex that recurs frequently
- New onset pelvic floor pain that interferes with daily activities
For mild discomfort without warning signs, scheduling an appointment when convenient is reasonable. Most women experience some pelvic pain during pregnancy or menstrual cramps that don’t require urgent evaluation unless the pain becomes debilitating.
Treatment Options for Pelvic Pain
When pelvic pain has an identifiable cause, treatment focuses on addressing the underlying condition. The approach varies depending on whether the pain is acute, chronic, or related to specific health concerns.
Treating Menstrual-Related Pelvic Pain
For pelvic pain in women tied to the menstrual cycle (such as cramps or endometriosis), doctors often recommend:
- Hormonal treatments – Birth control pills, patches, or IUDs to regulate cycles
- NSAIDs – Ibuprofen or naproxen for inflammation and lower abdominal pain
- Alternative therapies – Heat application, acupuncture, or hypnosis for refractory cases
Managing Chronic Pelvic Pain
For persistent chronic pelvic pain syndrome, a multidisciplinary approach often works best:
- Specialized medications – SNRIs or nerve pain drugs like gabapentin (opioids are rarely recommended)
- Physical therapy – Targeted exercises for pelvic floor pain or muscle tension
- Psychological support – Cognitive-behavioral therapy for pain management
- Surgical options – Laparoscopy for endometriosis or cyst removal in severe cases
Musculoskeletal Pain Relief
When pelvic girdle pain stems from muscle or joint issues:
- Rest and activity modification
- Heat therapy for muscle relaxation
- Targeted physical therapy for pelvic bone pain
Special Considerations for Older Women
Postmenopausal women often experience different causes of pelvic pain symptoms due to hormonal changes:
Common Causes in Older Women
- Urinary issues – Frequent UTIs causing lower abdominal pain after sex or urination
- Digestive changes – Constipation leading to lower abdominal pain before bowel movement
- Genitourinary syndrome – Vaginal dryness and urinary symptoms
- Reproductive cancers – Ovarian or endometrial cancer concerns
Important Warning Signs
Older women should seek prompt medical evaluation for:
- Any postmenopausal bleeding
- Unexplained weight loss
- Sudden digestive changes with lower abdominal pain and nausea
- Persistent bloating or pelvic pain location changes
Treatment Approaches
For age-related pelvic discomfort:
- Vaginal moisturizers or low-dose estrogen therapy for dryness
- Pelvic floor rehabilitation for chronic pelvic pain syndrome-like symptoms
- Thorough cancer screening when indicated
Final Thoughts
Pelvic pain can significantly impact quality of life, but understanding its causes and treatment options empowers women to seek appropriate care. Whether dealing with chronic pelvic pain syndrome, pelvic pain during pregnancy, or age-related discomfort, early intervention is key. By recognizing warning signs and working with healthcare providers, women can find relief and improve their daily wellbeing. Always consult a doctor for persistent or severe pain to rule out serious conditions and develop a personalized management plan.
Frequently Asked Questions
What causes sudden stabbing pain in the pelvic area in females?
Sudden sharp pain may indicate ovarian cyst rupture, ectopic pregnancy, or appendicitis. Seek emergency care if accompanied by fever or dizziness.
Can pelvic floor pain be treated without surgery?
Yes. Physical therapy, relaxation techniques, and medications often effectively manage pelvic floor pain without invasive procedures.
Why do I have lower abdominal pain after sex?
Possible causes include UTIs, Pelvic Infections, endometriosis, or muscle tension. Persistent pain warrants a gynecologic evaluation.
How can I relieve pelvic girdle pain during pregnancy?
Support belts, prenatal yoga, and warm compresses help. Severe pelvic girdle pain during pregnancy may require physical therapy.
When should chronic pelvic pain be evaluated?
If pain lasts >6 months, interferes with daily life, or is paired with bleeding/weight loss, consult a specialist.
Is lower abdominal pain before bowel movement normal?
Occasional mild discomfort may occur, but frequent pain could signal IBS, constipation, or inflammatory bowel disease.