Fibroids in the Uterus: Causes, Symptoms and Treatment Options
Fibroids, also known as uterine fibroids or leiomyomas, are non-cancerous growths that develop in or around the uterus. These growths vary in size, some may be as small as a pea, while others can grow as large as a melon. While many women with fibroids in the uterus experience no symptoms, others may face challenges like heavy menstrual bleeding, abdominal swelling, or urinary issues.
How Common Are Uterine Fibroids?
Fibroids are extremely common, though exact numbers are hard to determine since many women don’t experience noticeable symptoms of uterine fibroids. Research suggests that at least half of all women will develop one or more fibroids in their lifetime, with many cases occurring between ages 30 and 50. Genetics may play a role, as fibroids can run in families. Some women have a single fibroid, while others develop multiple growths of varying sizes.
Certain groups are more likely to develop fibroids:
- African American women have a higher risk, often experiencing larger fibroids at a younger age with more pronounced symptoms.
- Overweight women are also more susceptible, likely due to higher estrogen levels linked to excess body weight.
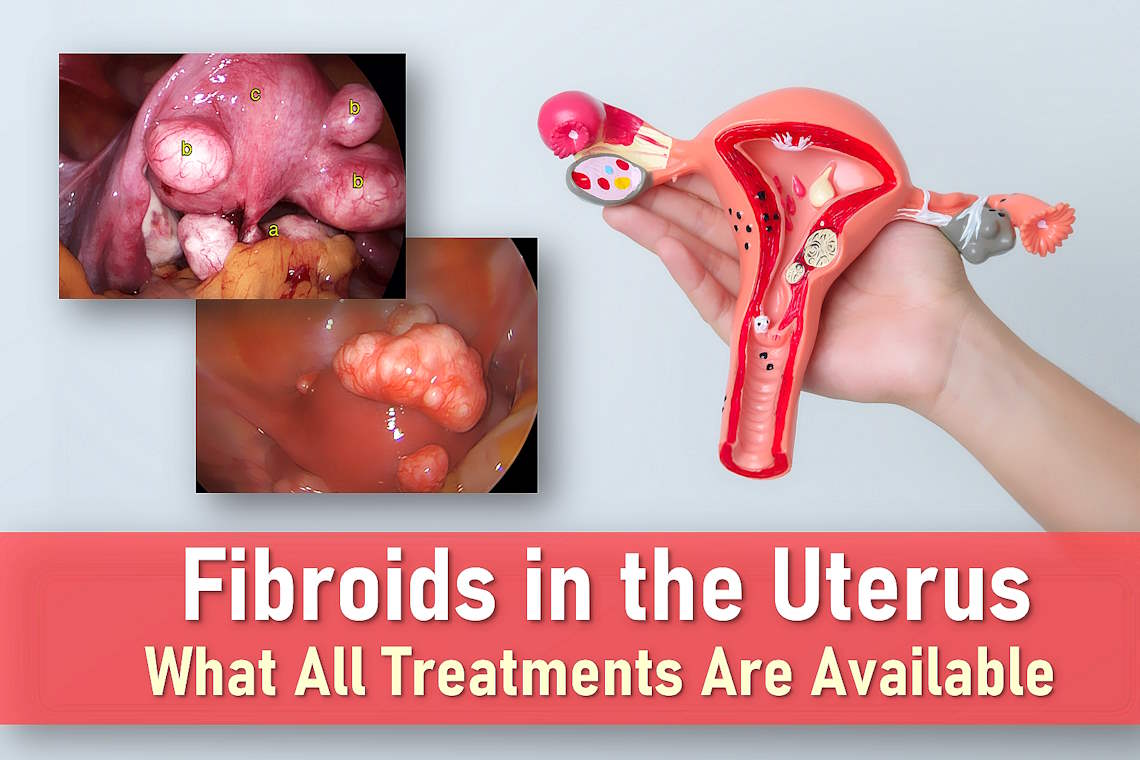
Fibroids can change over time, they may grow larger, shrink, or even disappear on their own. Their location in the uterus also varies, leading to different classifications:
Types of Fibroids
- Intramural fibroids: The most common type of fibroid, intramural fibroids grow within the muscular wall of the uterus. They can sometimes enlarge enough to stretch and expand the uterus, potentially causing discomfort, pressure, or changes in menstrual flow.
- Subserosal fibroids: These fibroids develop on the outer surface of the uterus and extend into the pelvic cavity. Subserosal fibroids can grow quite large, sometimes pressing on surrounding organs like the bladder or bowel, leading to symptoms such as urinary problems or constipation.
- Submucosal fibroids: These fibroids grow just beneath the inner lining of the uterus and protrude into the uterine cavity. Although less common than other types, submucosal fibroids are more likely to cause heavy menstrual bleeding, prolonged periods, and fertility challenges.
- Pedunculated fibroids: A type of subserosal or submucosal fibroid, pedunculated fibroids are attached to the uterus by a thin stalk (or stem). Depending on their location, these fibroids can cause pain, particularly if the stalk twists, cutting off the blood supply to the fibroid (a condition known as fibroid torsion).
Symptoms of Uterine Fibroids
Many women with fibroids in the uterus experience no symptoms at all. Often, fibroids are discovered incidentally during a routine pelvic exam or an imaging scan performed for another reason. However, when symptoms do occur, they can vary depending on the size, number, and location of the fibroids. Here are some common signs of fibroids to be aware of:
Heavy or Painful Periods
While fibroids don’t disrupt the menstrual cycle, they can cause heavier bleeding (fibroids symptoms often include prolonged or excessive periods) and more severe cramping. Over time, this blood loss may lead to iron deficiency or anemia, which can be confirmed with a blood test and treated with iron supplements.
Abdominal Discomfort and Swelling
Large fibroids may cause a noticeable bloating or fullness in the lower abdomen, similar to the sensation of weight gain. Some women also report persistent lower back pain linked to their fibroids.
Bladder and Bowel Pressure
If a fibroid presses against the bladder, it can increase urinary frequency or urgency. In rare cases, pressure on the rectum may lead to constipation.
Pain During Intercourse
Fibroids located near the cervix or vaginal canal can cause discomfort or pain during sex, a symptom that should always be discussed with a healthcare provider.
Reproductive Challenges
Though uncommon, fibroids, especially those that distort the uterine cavity, may contribute to fibroids and pregnancy complications, such as:
- Infertility: Rarely, fibroids block the Fallopian tubes or interfere with embryo implantation.
- Miscarriage: Very occasionally, fibroids may increase the risk of pregnancy loss.
- Pregnancy complications: Most women with fibroids have healthy pregnancies, but large or strategically located fibroids may raise the likelihood of breech positioning, preterm labor, or the need for a cesarean delivery.
During pregnancy, some women experience temporary fibroid-related pain if the growth outpaces its blood supply or twists on its stalk (a condition called “torsion”). If you’re pregnant and have fibroids, your doctor will monitor you closely to manage any risks.
What Causes Fibroids?
Fibroids develop from an overgrowth of smooth muscle cells and other tissue in the uterine lining. While the exact cause remains unclear, research shows these growths respond to estrogen and progesterone – the primary female hormones produced by the ovaries. This hormonal connection explains why:
- Fibroids often enlarge during pregnancy when hormone levels peak
- They typically shrink after menopause as hormone production declines
- Hormone replacement therapy (HRT) may delay this natural shrinkage
Diagnosing Uterine Fibroids
Doctors typically diagnose fibroids through:
- Pelvic exam: Larger fibroids may be detectable during a manual examination
- Ultrasound: The primary imaging tool to confirm diagnosis and rule out other conditions
- Blood tests: Often recommended for women with heavy periods to check for anemia
Fibroids Treatment Options
Not all fibroids require treatment. Many women with mild symptoms of uterine fibroids choose to monitor their condition, especially since fibroids often shrink after menopause. However, if symptoms worsen, these treatment options may help:
Uterine Fibroids Medication
For women with smaller fibroids and heavy bleeding, these uterine fibroids medication treatment options may provide relief:
- Tranexamic acid: Reduces menstrual bleeding by helping blood clots stay intact (taken during your period)
- Anti-inflammatory drugs (ibuprofen, mefenamic acid): Decrease prostaglandin production to lighten bleeding and ease cramps
- Birth control pills: The combined pill often reduces menstrual flow and pain
- Progestogen therapy: Available as pills, injections, or the levonorgestrel IUD (LNG-IUS) to thin the uterine lining
Note: The LNG-IUS may be difficult to place in women with larger fibroids, and progestogen injections may stop periods altogether.
Medications to Shrink Fibroids
For women seeking new treatment for fibroids without surgery, several medication options can help reduce fibroid size and alleviate symptoms:
GnRH Analogues
Gonadotropin-releasing hormone (GnRH) analogues like goserelin and leuprorelin acetate temporarily lower estrogen levels, causing fibroids to shrink. While effective for:
- Reducing heavy bleeding
- Relieving pressure symptoms
These medications create artificial menopause, potentially causing hot flashes and increasing osteoporosis risk. Therefore, treatment is typically limited to 6 months. Doctors often prescribe them for 3-4 months before surgery to make fibroid removal easier.
GnRH Antagonists
GnRH antagonists like elagolix, relugolix, and linzagolix have been shown to reduce bleeding and shrink fibroids. These medications work by reducing the release of hormones that control the production of estrogen and progesterone by the ovaries. Linzagolix is approved by both the FDA and the EU for up to 24 months of use with hormonal add-back therapy.
Progesterone Blockers
Ulipristal acetate (UPA) works differently by blocking progesterone’s effects – this hormone plays a key role in fibroid growth. By inhibiting progesterone, UPA can effectively shrink fibroids.
Combination Therapy
The FDA-approved medication relugolix-estradiol-norethisterone acetate offers a balanced approach for moderate to severe symptoms:
- Relugolix (GnRH antagonist) shrinks fibroids
- Estradiol minimizes menopausal side effects
- Norethisterone prevents uterine lining thickening
This oral medication preserves fertility while effectively reducing bleeding with fewer side effects than traditional options.
Surgical Treatments for Uterine Fibroids
Myomectomy
For women wanting future pregnancy, this uterus-sparing procedure removes fibroids via:
- Abdominal incision
- Laparoscopy
- Hysteroscopy (through the vagina)
While preserving fertility, there’s about a 30% recurrence rate. Surgeons may need to convert to hysterectomy if bleeding becomes uncontrollable during the procedure.
Hysterectomy
The most definitive solution for symptomatic fibroids involves womb removal through:
- Traditional abdominal incision
- Laparoscopic (keyhole) surgery
- Vaginal approach (leaving no visible scars)
This permanent solution is ideal for women who’ve completed childbearing.
Uterine Artery Embolization (UAE)
This minimally-invasive alternative performed by interventional radiologists:
- Blocks blood flow to fibroids via catheter-guided particles
- Shrinks fibroids over 6-9 months
- Shows symptom improvement within 3 months for most women
About 30% of patients require additional treatment later. UAE preserves the uterus while effectively treating symptoms.
Minimally Invasive Fibroid Treatments
For women seeking alternatives to major surgery, several advanced procedures can shrink or remove fibroids with less recovery time:
Myolysis Techniques
These procedures target fibroids directly to shrink them:
- Endometrial ablation: Destroys the uterine lining using laser, heated wire, or microwave energy – best for fibroids near the inner womb surface
- MRI-guided focused ultrasound: Uses concentrated sound waves to break down fibroids non-invasively (long-term fertility effects still being studied)
- Ultrasound-guided HIFU: Similar approach using ultrasound imaging for precision
Morcellation Procedures
These techniques break fibroids into smaller pieces for removal:
- Laparoscopic power morcellation: Allows fibroid removal through small incisions
- Hysteroscopic morcellation: Removes submucosal fibroids through the vagina
Important safety note: Morcellation carries risks and is generally not recommended for women over 50 or postmenopausal due to potential complications.
Potential Complications of Fibroids
While many fibroids cause no issues, possible complications include:
- Anemia from prolonged heavy bleeding, which may lead to fatigue, weakness, and shortness of breath if left untreated.
- Urinary problems like frequent urinary tract infections (UTIs), urinary urgency, or retention, often caused by pressure on the bladder from large fibroids.
- Reproductive challenges (rare but possible), such as difficulty conceiving or an increased risk of infertility, depending on the size and location of the fibroids.
- Pregnancy complications including miscarriage, preterm labor, abnormal fetal positioning, or the need for a cesarean section due to obstruction or pressure from fibroids.
- Fibroid torsion causing sudden, severe pelvic pain if the fibroid twists on its stalk, cutting off its blood supply and leading to a medical emergency.
- Fibroid degeneration occurs when a fibroid outgrows its blood supply. This can cause sharp, sudden, and severe pain, often accompanied by fever and abdominal bloating. These symptoms may persist for days or even weeks as the fibroid tissue breaks down and is reabsorbed by the body.
Long-Term Outlook for Fibroids
The progression of fibroids varies greatly from person to person, depending on factors like age, hormonal status, and overall health. Here’s what to expect over the long term:
- Most fibroids shrink naturally after menopause due to the natural decline in estrogen and progesterone levels. As hormone levels decrease, fibroids tend to reduce in size and symptoms often improve.
- Hormone replacement therapy (HRT) may slow this shrinkage process by maintaining higher levels of estrogen, which can stimulate fibroid growth in some cases.
- Some fibroids may reduce in size before menopause, especially in response to certain treatments or natural hormonal fluctuations, but this is not guaranteed.
- Symptoms often improve with treatment, including medications, lifestyle changes, or surgical options, depending on the severity of the fibroids and individual needs.
Regular monitoring through pelvic exams or imaging, such as ultrasounds or MRIs, helps track changes in fibroid size and symptoms over time. This allows healthcare providers to determine whether continued observation, medical management, or further intervention is necessary.
Frequently Asked Questions About Uterine Fibroids
What are the most common symptoms of fibroids?
The most frequent symptoms of uterine fibroids include heavy menstrual bleeding, pelvic pressure, frequent urination, and pain during sex. About 30% of women experience noticeable symptoms.
Can fibroids turn into cancer?
No, fibroids are almost always benign. The chance of a fibroid being cancerous (leiomyosarcoma) is less than 1 in 1,000 cases. However, symptoms of uterine fibroids and cancer can sometimes overlap, so proper diagnosis is important.
How can I check for fibroids at home?
While you can’t definitively diagnose fibroids in uterus yourself, you can watch for signs of fibroids like pelvic heaviness, bloating that doesn’t improve with bowel movements, or changes in menstrual flow. Always consult a doctor for proper diagnosis.
What foods help shrink fibroids naturally?
Some studies suggest foods for shrinking fibroids may include green leafy vegetables, flaxseeds, and foods rich in vitamin D. While diet may help manage symptoms, medical treatment is often needed for significant reduction.
Can you get pregnant with fibroids?
Yes, many women with fibroids and pregnancy have successful pregnancies. However, location matters – submucosal fibroids may affect fertility more than other types. Consultation with a specialist is recommended.
Final Thoughts
While fibroids are extremely common, they affect each woman differently. From lifestyle adjustments to medical interventions, numerous fibroids treatment options exist to manage symptoms effectively. Remember that symptoms like heavy bleeding or pelvic pressure shouldn’t be ignored – timely consultation with your healthcare provider can help determine the best approach for your individual situation. With proper management, most women find significant relief and maintain excellent quality of life.