Normal Vaginal Delivery – Stages, Tips & Complications
Vaginal delivery, commonly referred to as normal delivery, is the process where a baby is born through the vaginal canal. This natural method of childbirth is recommended for its many health benefits for both mother and baby. According to the National Institutes of Health (NIH), most women can safely undergo vaginal delivery, although some may face complications requiring a cesarean section (C-section). The childbirth journey, which begins with labor, is unique for every woman, and many opt for childbirth classes to prepare for this experience.
Benefits of Vaginal Delivery
Vaginal delivery has numerous advantages over a C-section. According to the American College of Obstetricians and Gynecologists, women who give birth vaginally usually have shorter recovery times, fewer infections, and less time spent in the hospital. Babies born vaginally often have fewer respiratory complications as well. These benefits make vaginal delivery a healthier option for both mother and child.
Am I a Candidate for Normal Vaginal Delivery?
If you’ve had a healthy pregnancy free of significant complications, you are likely a candidate for vaginal delivery. If you have previously had a vaginal birth, this further increases the likelihood. However, certain conditions, such as multiple pregnancies (twins, triplets), a breech baby, or a history of C-sections, may require your doctor to recommend a cesarean birth instead.
Pregnancy typically lasts 40 weeks, measured from the first day of your last menstrual period. Term pregnancies are considered those between 37 and 42 weeks, while preterm deliveries occur before 37 weeks, and post-term deliveries happen after 42 weeks. Around 80% of women deliver between 37 and 42 weeks, while about 11% experience preterm births.
Initiating Labor
Labor often begins within two weeks of the estimated due date. The onset of labor is believed to be influenced by mechanical and hormonal factors, although the exact cause remains unclear. For first-time mothers, labor typically lasts 12 to 18 hours, while subsequent deliveries may only take 6 to 8 hours. Simple activities like standing and walking during early labor can shorten this time by over an hour.
Signs of Labor Onset
It’s important to recognize the signs of labor, which include:
- Regular contractions in the lower abdomen
- Lower back pain
- The appearance of a “bloody show” (discharge of mucus mixed with blood)
- Rupture of membranes (“water breaking”)
Women with a history of rapid deliveries should contact their doctor as soon as contractions begin. Early contractions may feel mild and irregular, similar to menstrual cramps, but they will intensify and become more regular as labor progresses.
Stages of Labor and Delivery
Labor is divided into three main stages, each playing a crucial role in the birthing process:
First Stage: Labor Initiation and Progression
This stage is further divided into two phases: the initial (latent) phase and the active phase.
- Initial (Latent) Phase: Contractions begin mildly and become stronger and more rhythmic. The cervix starts to dilate, reaching approximately 4 centimeters. This phase may last 8 to 20 hours for first-time mothers and 5 to 12 hours for those who have previously given birth.
- Active Phase: Contractions become more intense, and the cervix dilates from 4 to 10 centimeters. This phase typically lasts 5 to 7 hours for first-time mothers and 2 to 4 hours for subsequent deliveries.
Second Stage: Baby Delivery
The second stage begins when the cervix is fully dilated and ends with the birth of the baby. This stage usually lasts 1 to 2 hours for first-time mothers and about 1 hour for subsequent deliveries. If pain relief such as an epidural has been administered, this stage may take longer.
Third Stage: Placenta Delivery
The third and final stage involves delivering the placenta. This usually happens within a few minutes but may take up to 30 minutes. After the baby is born, mild contractions help separate the placenta from the uterus.
Managing Ruptured Membranes
If your water breaks before labor begins, it’s essential to contact your healthcare provider. Labor typically starts within 24 hours. If not, induction may be necessary to reduce the risk of infection.
When to Go to the Hospital
You should head to the hospital or birthing center if:
- Your water breaks
- Contractions occur regularly, at intervals of 6 minutes or less, and last at least 30 seconds
- You have significant cervical dilation (over 4 centimeters)
Upon admission, doctors will monitor your contractions and assess the baby’s position. A favorable position for birth is when the baby’s head is down, facing the mother’s back, with the chin tucked and arms folded.
Fetal Monitoring
Fetal heart monitoring is essential during labor to ensure the baby’s well-being. External or internal monitoring tracks heart rate patterns and can indicate if the baby is in distress, requiring immediate medical intervention.
Pain Relief Options
You may choose from several pain relief options during labor:
- Natural Childbirth: Relaxation and breathing techniques to manage pain
- Analgesics: IV medications such as fentanyl or morphine
- Local Anesthetics: Numbing the vaginal area with a pudendal block
- Regional Anesthesia: Epidural or spinal injections for comprehensive pain relief
- General Anesthesia: Usually reserved for emergency C-sections
The choice of pain relief depends on your preferences and your healthcare provider’s recommendations.
Natural Childbirth Techniques
Natural childbirth emphasizes conscious coping strategies, including relaxation and breathing exercises. Childbirth classes can help you master these techniques.
- Relaxation: Focuses on releasing tension during contractions
- Breathing: Different breathing patterns are used to manage the intensity of contractions
Support from your partner or healthcare team is critical during labor.
Delivery Process
The delivery process varies depending on the baby’s position and your labor progression. The healthcare provider may use instruments like forceps or a vacuum if assistance is needed. Episiotomies are no longer routinely performed and are only done when necessary.
Placenta Delivery
After the baby is born, mild contractions help the placenta detach from the uterus. In most cases, it is delivered naturally within 3 to 10 minutes. Healthcare providers will ensure that the placenta is completely expelled to avoid postpartum complications.
Post-Delivery Care
After delivery, oxytocin may be administered to contract the uterus and minimize blood loss. Your healthcare provider will check for any vaginal tears and repair them if necessary. Immediate skin-to-skin contact between mother and baby is encouraged, and breastfeeding is often initiated within the first hour.
Common Complications During Normal Delivery
1. Fetal Meconium
If the amniotic fluid appears greenish or brown rather than clear, it may indicate fetal meconium, which can signal distress. Meconium is normally passed after birth as the baby’s first bowel movement, but its presence in the amniotic fluid requires immediate medical attention.
2. Abnormal Fetal Heart Rate
The fetal heart rate is a strong indicator of how well the baby is coping with labor. A normal heart rate is between 120 and 160 beats per minute. If the baby shows signs of distress, oxygen, IV fluids, or changes in the mother’s position can help.
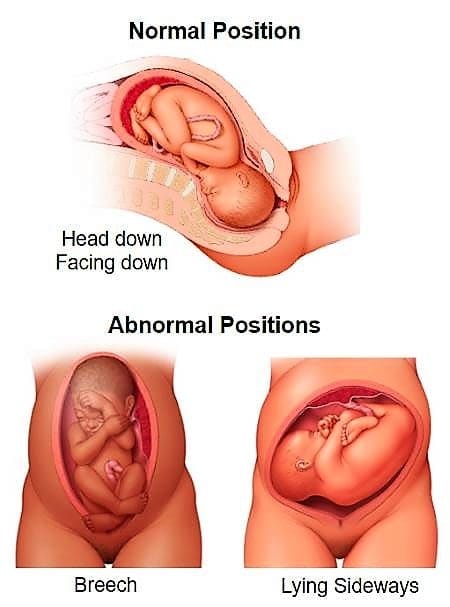
3. Abnormal Baby Positions
Several abnormal positions can make delivery more difficult, including:
- Face Presentation: The baby’s face is positioned to enter the birth canal first.
- Breech Presentation: The baby’s buttocks or feet are positioned to come out first.
- Transverse Lie: The baby is lying sideways, making vaginal delivery impossible.
Your healthcare provider may attempt to turn the baby or recommend a C-section if necessary.
4. Vaginal Bleeding and Tears
Some blood loss during delivery is normal, but excessive bleeding can pose a risk. Severe tears during delivery are not always preventable, but immediate medical intervention helps minimize complications.
Post-Delivery Recovery
Recovery after a normal delivery is generally quicker than after a C-section, but there are still important guidelines to follow. If you experience tears, keep the area clean and avoid baths or swimming for six weeks. Contact your doctor if you notice large blood clots, have trouble urinating, or experience fever or tenderness in the uterus. By adhering to these guidelines and maintaining regular check-ups, you can ensure a smooth postpartum recovery.










